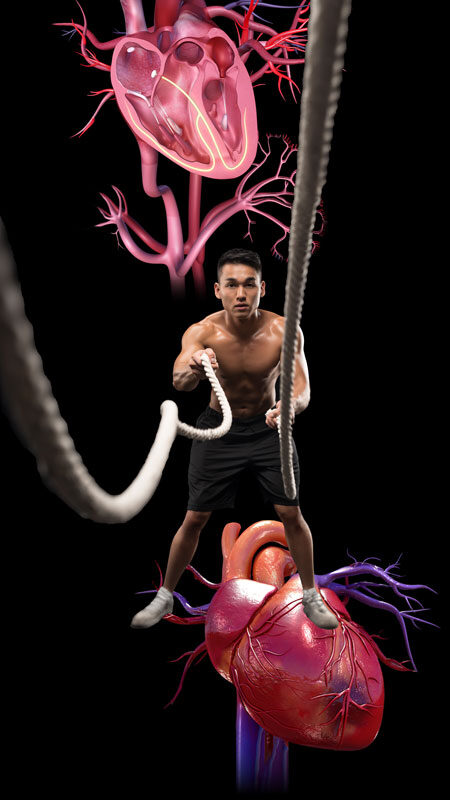
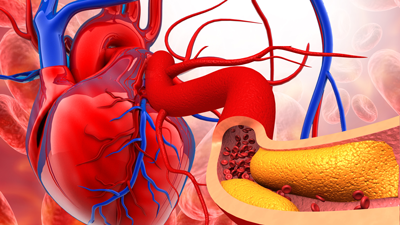
Our heart is our body’s engine, it’s what keeps the blood circulating so it can transport all the nutrients that our different body parts depend on, and so that it can remove all the waste. Caring for our heart should be a top priority for all of us. Sadly, heart disease is the number one cause of death in the world.
The good news is that a large amount of these deaths are preventable if we follow a healthy diet and adopt good lifestyle habits like getting proper sleep and exercising. The sad news is that most people are still following the Standard American Diet (SAD) which is packed with saturated fat, cholesterol, sodium and toxins, and low in fiber.
The scariest part is that most children are already developing heart disease, due to diets packed with saturated fats and sodium. It takes years to build up, so it typically doesn’t manifest until they’re older. Fad diets promoting animal-based products while antagonizing healthy carbs are worsening this situation.
Below, we talk about how our heart works, the nutrients that support it, and some of their top plant-based sources. We also share important facts that can help you take great care of your heart and your family’s precious hearts.
Hover over each pointer to discover what makes our heart beat and to go over the main parts of our heart and their different functions.
Click on the nutrient images below to visit their interactive pages and learn more about what they do for us, their top sources, other interesting facts, and to try our personalized nutrition calculators.
Fiber
Protein
Vitamin A
Thiamin or Vitamin B1
Pyridoxine or Vitamin B6
Folate or Vitamin B9
Cobalamin or Vitamin B12
Ascorbic Acid or Vitamin C
Vitamin E
Vitamin K
Calcium
Iron
Magnesium
Selenium
Potassium
Below you can see some of the top whole-foods, plant-based nutrient sources for our heart. Hover over each one to see their top heart-related nutrients, or click on it to visit its interactive page with a personalized calculator to help you identify all the nutrients this food provides. You will also find tips to help you select, store, and prepare these foods. Plus, you will get more important information on how this food can benefit your health and the health of your loved ones. For additional sources per nutrient, click on the nutrients above.

Beans and Legumes
Rich in vitamins B1, B6 and B9 (folate), calcium, iron, magnesium and selenium.

Dark Leafy Greens
Rich in vitamins A, B6, B9 (folate), C and K plus calcium, iron and magnesium.

Whole Grains
Rich in fiber, vitamins B1 and B6, iron, magnesium & selenium.

Walnuts
Rich in vitamin B6, magnesium, and phytonutrients that may cut our risk of dying of heart disease by half.

Edamame
Rich in calcium, iron, magnesium, potassium, and vitamins B1, B9 (folate) and K.

Sweet Potato
Rich in vitamins A, B6 and C, and in potassium.

Asparagus
Rich in vitamins B1, B9 (folate), C, E and K, and in potassium and selenium.

White Mushrooms
Rich in iron, potassium, and selenium.

Steve Walsh was an amazing father and human being who lived life with compassion, unconditional love, a strong dedication to justice, and a great sense of humor. He died from sudden cardiac arrest at the early age of 62. This page is dedicated to him, hoping that the information we provide helps other families prevent this tragic loss.